1 in 31 hospital patients has at least one healthcare-associated infection (HAI) on any given day. The 2018 National and State HAI Progress Report provides data on central line-associated bloodstream infections (CLABSIs), catheter-associated urinary tract infections (CAUTIs), ventilator-associated events (VAEs), surgical site infections (SSIs), methicillin-resistant Staphylococcus aureus (MRSA) bloodstream events, and Clostridioides difficile (C. difficile) events, formerly known as Clostridium difficile.
Ventilator-Associated Events
Ventilator-associated events are tracked nationally based on data collected from Acute Care Hospitals (ACHs) and Long-Term Acute Care Hospitals (LTACHs). Between 2017 and 2018, there wasn’t any statistically significant change in these reported events. Among these events, ventilator-associated pneumonia (VAP) is the most serious and controversial of the infections of critically ill patients. (1)
Ventilator-associated pneumonia is defined as pneumonia that occurs 48-72 hours or thereafter following endotracheal intubation, characterized by the presence of a new or progressive infiltrate, signs of systemic infection (fever, altered white blood cell count), changes in sputum characteristics, and detection of a causative agent VAP contributes to approximately half of all cases of hospital-acquired pneumonia VAP is estimated to occur in 9-27 % of all mechanically ventilated patients, with the highest risk being early in the course of hospitalization. It is the second most common nosocomial infection in the intensive care unit (ICU) and the most common in mechanically ventilated patients. The complex interplay between the endotracheal tube, presence of risk factors, and the virulence of the invading bacteria and host immunity largely determine the development of VAP. (2)
The American Thoracic Society, in conjunction with the Infectious Disease Society of America, published a guideline for the management of this particular healthcare-acquired infection. This evidence-based guideline outlines early and appropriate treatment with antibiotics. They also stress avoiding excessive antibiotics and ramping down antibiotic therapy based on microbiological cultures. (3)
Catheter-Associated Urinary Tract Infections
According to the CDC, when a urinary catheter is not put in correctly, not kept clean, or left in a patient for too long, germs can travel through the catheter and infect the bladder and kidneys. This type of healthcare-associated infection (HAI) is called catheter-associated urinary tract infection (CAUTI). This type of infection causes the “revolving door” of hospital re-admissions that costs the health care system nearly $4 billion dollars annually. This leads to antibiotic use which in turn leads to colonization of multi-drug resistant organisms. (4)
Educating facility staff (5) was key to reducing infection rates by about 40%. (6) This, in turn, caused a reduction in the frequency of lab tests being ordered. Too much testing can lead to false-positive results and the use of unnecessary antibiotics, which can encourage drug-resistant superbugs to evolve and spread.
As long-term care facilities implemented practices to reduce infection, the rate dropped from 6.4 infections per 1,000 catheter-days to 3.33. This can help reduce health care costs across the board. The US Department of Veterans Affairs and others funded an online calculator to estimate the costs of CAUTIs.
In Conclusion
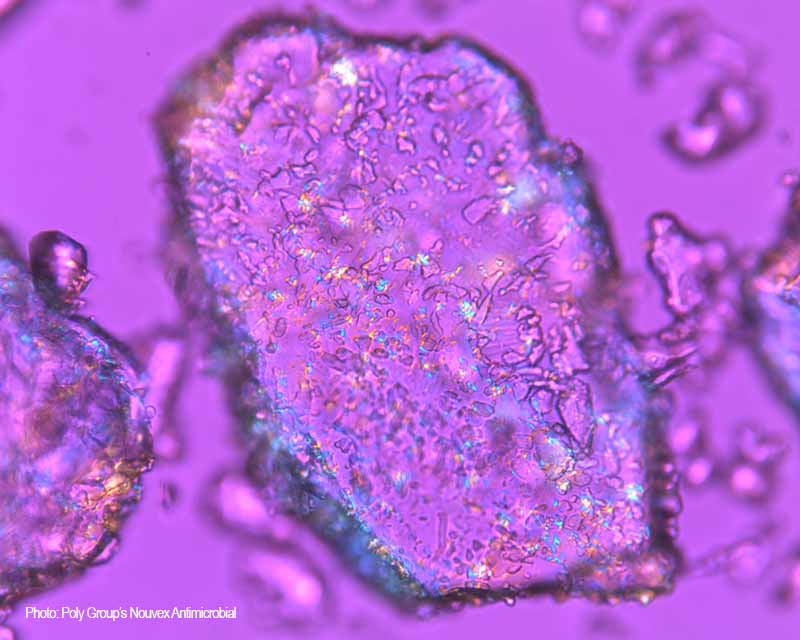
Healthcare-associated infections are a serious healthcare issue. If you are a medical device manufacturer or durable medical equipment manufacturer that would like to incorporate an antimicrobial into your polymer, we urge you to Contact Us to discuss this data in further detail. If you would like to stay up to date about PolyGroup and Nouvex Antimicrobial, please subscribe to our newsletter.